Talk for the Islington U3A on 19th September 2019, under the heading: The NHS is 71 –should it retire?
Introduction
I was invited to give this talk shortly after I’d heard yet again (and at a U3A event) the phrase ‘creeping privatisation of the NHS’. As always I’d ignored it at the time but I thought I’d take this opportunity to explore that. To suggest that while a stealthily creeping anything would be a worry, privatisation isn’t the main concern. There is a much bigger one, and that’s been as much a feature of Labour as of Tory governments.
I want to look at what has been going on in the NHS and in wider society; how that’s affected the kind of care that is on offer; contrast that with the kind of care we want and need; and then look at the options open to us about the shape of our national health system.
I’m approaching this, not from a health policy standpoint, nor that of an historian. My interest for the last 40 years has been in behaviours and dynamics within the NHS, with a particular interest in status differences and how those affect decision making.
I’ll start by looking very briefly at what I see as some seminal moments in the history of the NHS since the 1960s, then at the background forces influencing these, at how where we are today is hugely suboptimal, and at what other ways forward could offer. I’m hoping to interest and energise you, and expecting along the way to irritate you!
Seminal moments in NHS history
The Salmon Report on Nursing 1967
This was the end of the Hattie Jacques stereotype: the matron very much in charge of a ward was replaced by a much clearer nursing career structure with every hospital having a Chief Nursing Officer. This was responding to changing expectations and attitudes of young women.
(In passing, I think its worth remembering that the nursing professions had been profoundly influenced by the first world war and the number of intelligent, educated young women who now had no chance of a family life and for whom nursing was much more than a job and an income. Sometimes I feel our expectations of nurses are still shaped by that very important part of its history and we can be more disappointed than we realistically should be by the nursing care offered to us).
This was a very sensible report, but every change always achieves losses as well as gains and its important to notice both, and here there was some loss of ownership and continuity at ward level.
The Griffiths report 1983
Roy Griffiths (chief executive of Sainsbury’s) proposed replacing the existing Management Teams of Medical Officer, Nursing Officer and Administrator with a single General Manager – because ‘if Florence Nightingale were to walk the corridors of the NHS today with her lamp she would be trying to find the person in charge’. In other words decision making was, he felt, slow and involved too many people. And his changes did indeed make decision making quicker, but with the loss of involvement of key players, so that critical issues were often not considered or understood.
What Griffiths never understood was that the NHS is an example of a ‘disconnected hierarchy’. Unlike Sainsbury’s where people can be told what to do, professional organisations like healthcare rely on professionals with a knowledge base they deploy at their own discretion. This gives them a status that enables them to (to a certain extent) choose whether and how to engage with the management of an organisation. The tripartite team recognised the reality of that, a management hierarchy does not.
The Purchaser- provider split 1991
Ken Clarke in Margaret Thatcher’s government divided NHS organisations into those providing services, and those deciding which services should be provided and by whom.
The gains were that information about health needs (and public health information more generally) played a much greater part in decisions about the range of services offered, BUT it has taken a long long time to develop effective ‘purchaser’ skills (arguably we still haven’t), because buying health services is very different from buying widgets, and it has diverted a lot of resources into the negotiating and contracting process.
This purchaser/provider split has been modified several times since then, most recently and fervently with the Lansley reforms of 2010. (This also swept away the Strategic Health Authorities that oversaw the wider operation of the NHS, and insisted that all contracts for services should be open to the private sector as well as NHS organisations).
The New GP contract 2008
GPs gave up their 24 hour responsibility for their practice population, and agreed to a public health agenda at every consultation in addition to the patient led one (e.g. Blood Pressure measured at every visit). This has had a positive impact on inequalities while also reducing the personal nature of the relationship.
Over this time period there were also some of what I call, in this age of acronyms, TMOs (Tragically Missed Opportunities!)
TMO 1: The Resource Management Initiative 1987
With the advent of personal computers this initiative aimed to give clinicians the information they needed and wanted to improve their clinical care. Because this had clinical benefits clinicians ensured excellent quality of the data entered. This would also allow better management of the whole hospital, but clinical care data took priority and management information was extracted from that. This was the EXACT OPPOSITE of the big NHS computer system that was a total failure in the early 2000s. The RMI was still a small scale experiment when the purchaser-provider split took place and was lost in that process.
TMO2: New Labour’s exciting amazing NHS targets
18 months to 18 weeks, 4 hours max in A and E. ………
The tragedy is that this could have the most exhilarating and worthwhile, life enhancing challenge: developing new and different and better ways of doing things. Instead it was a draconian and terrifying time for people with responsibility for these, ‘if you don’t deliver this target your job is on the line’, leading mostly to duplicating capacity and redefining activities or spaces.
But where are we today?
Sustainability and Transformation Partnerships 2016 – ongoing
STPs are a new kid on the block and have re-introduced a spirit of collaboration in place of competition. Local ‘accountable care systems’ are groupings of hospital, community, primary care and social care services with a single budget.
There are still only a few, and they depend on the goodwill of Boards and managers involved because their legal status is still as independent organisations. And there’s always the danger of things being rushed and muddled. But for the first time in a long time it feels like a sea change.
And a sea change is sorely needed – because what we’ve discovered in the last 30 years (although not everyone has noticed) is that a pretend or quasi market -the purchaser provider split- is not a half way house between a market and a centrally run system, with the benefits of each – but a completely different animal. If you have a pretend market you end up with a pretend everything else (pretend costs, accounting, management, quality, everything).
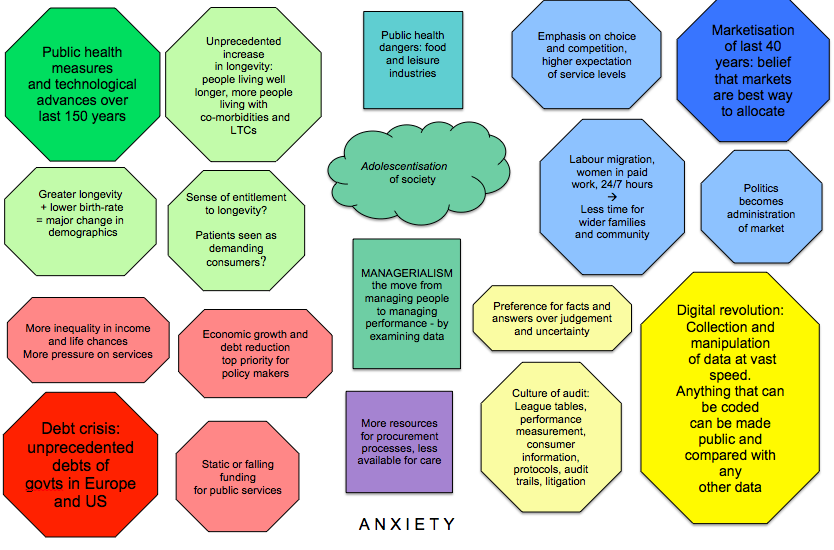
A key shift in the nature of management across society – and its consequences for health care
But we’ll come back to that, because something else has been going on in society over this same time period and unless we understand that we won’t get a sea change – we’ll get existing behaviours with new names. We need to get that out into the open, give it a name, and make it an explicit part of the decisions that are made.
In fact its got a name: an old name: MacDonaldisation.
This way of thinking is often attributed to Robert McNamara although I personally think it has much more to do with the increasing role and reach of Business Schools: its about the use of data to chart our progress towards a particular goal; about cutting through the noise of a complex and moving situation to work out what’s really going on and how you’re influencing it through your own actions: about identifying the critical interventions and key indicators of performance; finding ways of using sound logic to chart a way forward.
And surely that is what we want…..
Here’s an example: if you ask the CEO of any large charity they will tell you that their donors want to be sure that their money is being used to best effect, so they want to be kept informed about exactly how the money will be spent and what results that will have, how progress will be monitored, what performance indicators they can expect. The Gates Foundation is renowned for exactly this kind of rigour.
But not everyone sees this as a good thing.
John Ralston Saul wrote a book in 1993 called Voltaire’s Bastards: the dictatorship of reason in the West.
This management method, he said, is one ‘example of reason separating itself from, and out-distancing, the other …human characteristics of spirit, appetite, faith, emotion, intuition, will and experience’.
‘Voltaire’s ‘reason’ challenged the arbitrary absolute power of the aristocracy, Now the dictatorship of the absolute monarch has been replaced by that of absolute reason’.
More recently anthropologist Marilyn Strathern phrases it slightly differently: she talks of a culture of audit in which aspects that can be codified are privileged over those that cannot: ‘the vital wisdom drawn upon to inform an act is as important as the act itself but is not and cannot be captured’, so this leads to ‘hyperactivity and discourse being privileged over wisdom and silence’.
As a result, she suggests, professionals feel they are treated as a depersonalized unit of economic resource whose productivity and performance must be constantly measured and enhanced, instead of an autonomous practitioner making a valuable contribution to society through interpretive application of their expertise.
This is MacDonaldisation. At MacDonald’s everything can be measured (the height of the bun, the weight of the burger, temperature of the flame, perhaps even the width of the smiles!) and in situations where we can measure everything then data based logic like this works well. But, not everything can be measured…..
And here it’s time to look at a distinction made by systems thinkers in the 60s and 70s: a distinction between puzzles, problems and messes. A puzzle, suggested Russell Ackoff, is a situation where there is a right way forward and we can find out what that is; a problem doesn’t have a right way forward but some ways will be better than others and we can consult experts to see what they are. A mess, though, is very different, its a complex system of interacting problems and puzzles, and here we can only here take a step forward, see what happens, and then decide on our next step. This is technically called ‘muddling through’ and, when done well, ‘muddling through elegantly’!. This is what we need professionals for. This is where we need Aristotle’s ‘phronesis’, practical wisdom, knowing how rather than knowing that, having an ability to tolerate the uncertainty of that and to move forward knowing that you’re not sure.
As Strathern notes: Professionals are society’s way of dealing with uncertain situations and we must encourage professionals not to lose their concern for society and its members and become units of production.
If we are not to drive this out, we need to leave space for our professionals, so we ourselves need to stop demanding answers where there aren’t any.
If we insist on knowing ‘which is the best school?’, for example, we will get a completely meaningless league table – and the attention of school staff diverted from relating with our children to focusing on data points that affect their position on the table.
As Strathern notes ‘audit sounds neutral but it fundamentally alters the nature of what is being audited’.
We need to accept that sometimes we cannot know, we will have to make a judgment, and put in the work to make that judgment. Of course its our anxiety that fuels this. (We worry our children won’t do as well as they could). But we need to learn to contain that anxiety and not belch it out into the wider system.
So we need to recognise messes when we come across them. And support the people tackling them on our behalf. We need to support them too when things go wrong:
It was human but very dangerous for Ed Balls to dismiss Sharon Shoesmith in the House of Commons when one of her social workers made a decision and Baby P died. That and the associated headlines did great damage to the practice of social work and recruitment to the profession.
That was an example of what systems thinkers call ‘spurious retrospective coherence’: When we look backwards at something that has happened we find a pathway between an action and the event. But when looking forwards before the action there were many many pathways that might ensue and it is impossible to know which will take place. It is important here that people feel able to take a risk.
Public Inquiries of any kind almost inevitably fall prey to this spurious retrospective coherence. Bristol cardiac centre , Francis and Mid Staffs,…. They all too often result in diligent people who have been working hard in difficult circumstances finding themselves pilloried or sacked for doing their best. Tragedies happen, they aren’t always somebody’s fault, and the kind of things we ‘learn’ from these kind of Inquiries (their findings and recommendations) can also make life more difficult for people facing similar situations in the future. We have to treasure professional judgment and not drive it out with an insistence on pure reason.
How is this relevant for how we organise the NHS? There are two important points:
1.Many health needs, people’s lives, complex NHS organisations and all the interactions within and between these – are not puzzles. They are messes.
2. Griffiths and the purchaser/provider split were both examples of MacDonaldisation.
The kind of organisations needed in health care
I believe that it has been MacDonaldisation rather than privatisation that has taken us down the wrong track in the NHS. MacDonaldisation (and its offshoot the pretend market of the Purchaser/ Provider split) have distorted our healthcare organisations. We need to liberate them, get them back into a real world , and work with clinicians and their disconnected hierarchy not against that.
What would our healthcare organisations look like if we did that? Here are some of the key features.
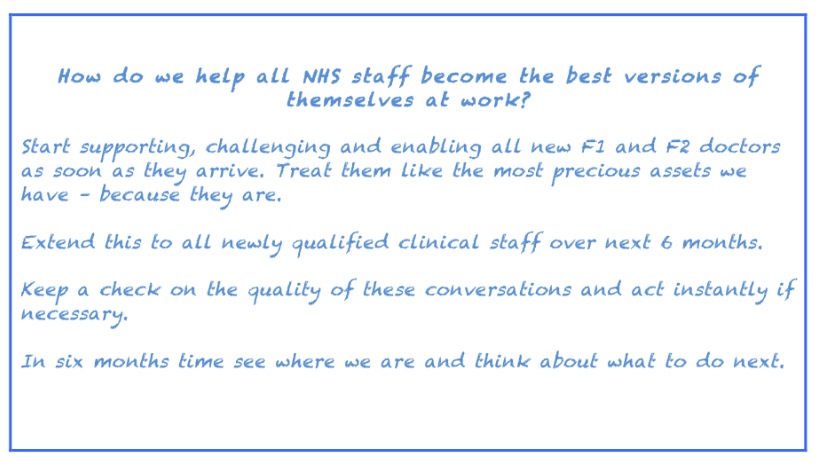
- Staff of all sorts would be being supported, challenged and enabled to do their best through ongoing conversations with their seniors (or peers for the most senior). In this way they would develop and maintain their ability to work with ‘messes’ as well as ‘puzzles’ and ‘problems’.
- The most junior staff (especially, but not only, doctors, nurses and therapists of all kinds) would be being well looked after, as the organisation recognised that these early days will influence their behaviour, confidence and performance over the next 40 years.
- Money would be being used wisely through a widespread understanding of costs and cost structures (fixed and variable costs, direct and indirect costs) and how changes in volume of activity, and changes to product mix or skill mix, all affect the ‘bottom line’. Only in this way do people know how to make savings, and how to invest new money wisely. In a pretend market using tariffs instead of real prices and costs this is impossible.
- Experienced members of an organisation would be contributing to strategic decisions about it. Clinical leaders, instead of being tasked to ‘win hearts and minds ‘ to a ‘compelling vision’ already developed by external consultants, would help their colleagues understand the complex reality of the challenges facing the organisation so that they can all contribute solutions and understand the reasons for the direction eventually chosen. Yes this is time consuming and expensive but not as expensive as big change programmes collapsing part way through their implementation.
- People in the organisation would be constantly keeping their eyes open for better ways of doing things, taking an interest in how patients experience their service, trying things out, seeing how patients react, offering genuinely different options about how care is delivered.
- Organisations would be demonstrating the same ambitions (for achieving optimal health) for all their patients regardless of diagnosis. For example being as ambitious for patients with schizophrenia as for those with cancer; for those with dementia as those with a heart attack or stroke. The NHS prides itself on making care available to all, but it doesn’t have the same ambitions for all. We need to reclaim the purpose of healthcare: it is not only about providing a set of auditable transactions in the form of a predesigned evidence based care pathway. It needs to be wider: my own definition of health care is ‘acts of work and courage in pursuit of flourishing’.
- Enough people in the organisation would have an understanding of how work flows through it: some basic knowledge of systems engineering enables people to design queues and waiting lists out of their local system. Calling for more money without that kind of analysis should be unethical.
- What it is that patients want and most value would be widely understood. Not through Patient representatives on Boards etc, nor ‘Friends and Family’ tests, nor Pat Sat questionnaires. But by (a) high quality ethnographic research about the kind of relationship people want to have with the NHS. Currently we have no idea- we make assumptions , we simply don’t know. (b) Using Citizens’ Juries for difficult decisions that are essentially political. For example decisions made by NICE are currently based on the seductively simple but philosophically questionable QALY, a Citizens Jury could replace that (as advocated by two Nobel Laureates Amartya Sen and Daniel Kahneman).
- And last but not at all least: there would be a range of effective treatments that are good Value For Money for the widest range of ill-health conditions. Currently we have sky high prices for lacklustre, me-too drugs , serving only lucrative diseases (leaving some orphaned and many underserved), and almost no research into non-pharmaceutical avenues of care. We urgently need a change in our method of funding innovation and research.
How to achieve a National Health System with organisations of this sort
So if that is the kind of organisation, the kind of energy and dynamics and behaviours we want in our health system, how can we get that?
Well we’ve given the Purchaser/Provider split a very very good go, and if even one of its designers, economist Alan Maynard, can say that it is ‘neither effective nor cost effective’ then we really must let it go. What can we choose from instead? I suggest that we can choose between an effective centrally run system and a carefully designed market. Let’s look at these.
An effective centrally run system
Let’s imagine a system directly and actively managed from the Department of Health. But perhaps managed isn’t the right word, because we do not want a return to the system we had before Ken Clarke’s purchaser-provider split. Instead we need to use something we didn’t have then: a plethora of relevant information from a range of different sources.
The role of the DH would be to gather, hold and provide, rich and relevant information from a wide range of sources to local healthcare organisations.
The information could include, for example, the NHS’s own (rather scattered) data, the rich data held by the tech giants, and that held by drug companies and other suppliers. It would need conversations with Big Tech to encourage them to make available their information about people’s needs and wants (on an aggregate and anonymised basis); also contracts with Big Pharma and other suppliers that ensure all research data is made available as part of their ongoing relationship with the NHS. And all of these would need to be supplemented by high quality research by anthropologists and sociologists and others into how people feel about different kinds of care in varying circumstances.
As well as gathering and providing data and information the DH would ask what uses these were being put to and how services were responding: being developed, altered, monitored, etc. Clinicians are much more likely to be inspired to design new and better services when given good information about what patients want and need than they are by targets set by managers, so we can imagine very different services emerging. In other words, robust varied information would act as the fuel that stops this large centrally held organisation from being a lethargic bureaucracy.
The DH could also encourage the sharing of information between organisations. For example information about costs and cost structures, and how product mix, staff mix, etc varies between services in different organisations and what impact this has on outcomes and satisfaction. Not in a command and control way – but an informative one, expecting and encouraging interest and enthusiasm.
In this process the boundaries between organisations may change as the information flows indicate more exchange of information (and hence activity) between some activities than others. In this way service redesign and hospital reconfigurations would be based, not on politics but on real activities rooted in real patient needs.
Instead of argument and insistence, this would lead to everyone becoming interested in the data and in how to improve services in the light of it. Even the thorny issue of the different status of different diagnoses (cancer v dementia for example) is likely to be addressed as information about the impact on the quality of lives is collected and not only on their length.
There would still be a need for making difficult decisions, for example those currently taken by NICE on the basis of the QALY, and in these areas Citizens Juries could be convened. indeed the DH could usefully develop an expertise in supporting such activities.
So the role of the DH would not be management as we have known it, it would be that of ensuring that information is available and used, that decision making processes involve the voices of people affected by them, and that political decisions are taken in genuinely political ways, remembering that the original Athenian democracy focused on discussion and increasing awareness of an issue and used a vote as only a last resort. In this way it would ensure that resources are being used wisely and well.
The Sustainable Transformation Partnerships could form part of this and lead into it.
Now lets look at another alternative.
A genuine but regulated market
Before we think any further about this lets remind ourselves that there are lots of different kinds of market and there is no need at all to adopt the kind of market we see in parts of the US system.
Let me tell you a story. About something that has been happening in the Netherlands.
A few years ago an ex-health finance manager, Jos de Bloc, set up an unusual community nursing team. It had no manager, the nurses themselves (together with their patients) took all the decisions about the best care for those patients, and managed their resources and their case loads themselves. This proved so popular with both patients and nurses that within a few years over 60% of the Netherlands had local teams offering this service, known as the Buurtzorg system.
How had Jos de Blok and his nurses achieved this degree of coverage in such a short time?
To set up a new team he needed to have 20,000 euros available. The team was set up, registered with relevant organisations and started offering its services. Patients liked this service more than others on offer and chose it. By the time his euros were running out money was flowing in from the insurance companies, the service was viable and he could set up another team elsewhere. In other words if the patients chose the service the system supported their choice
Many people in the UK are very interested in this system, commissioners, managers and nursing organisations are keen for it to be offered. Jos de Blok is keen to offer it here. His UK agents, Public World, are doing sterling work. But to date nothing like 60% coverage has been achieved. Why? Because the decisions are being made by commissioners and managers. Not patients. When patients can choose they make different decisions from managers.
Of course not all services are as easy to choose between as community nursing care but in a system where decisions are not tested with real patients we can never be sure whether we are meeting their needs and preferences.
The Netherlands used to have a system similar to ours but in 2006 it switched to a market system that they designed for themselves reflecting the values they considered the most important. The three they chose were access to care for all, solidarity through insurance which is compulsory, and high quality services.
It consists of two compulsory basic insurances that between them cover both the care we expect from our NHS and also long term care. These are paid for by a premium, set by the government, paid to a private insurance company. This is accompanied by an income-related payment from employers. People on low incomes can apply for a reduction in the basic premium. The private companies are not allowed to charge anyone a higher premium than agreed with the government, nor to reject an applicant.
(It is also possible to buy further insurance to cover additional aspects and for this the companies can charge what they like and can reject people they see as a bad risk).
I suggest that this is not hugely different in terms of financial contribution from that of residents in the UK, and that we would not notice a large difference to our personal finances if it were introduced here. And I am not suggesting that we adopt an identical scheme but that it would be possible to design one ourselves. I am merely observing that with their system patients are offered services they want more readily than here.
I believe we could valuably include a move to a market system that we design, again perhaps using Citizens Juries in the design process, in our options for a way forward.
Plus a different system for research and innovation
Neither of these options addresses the need for much more effective innovation resulting in a wide range of effective and reasonably priced health treatments. And that is still very much needed whichever system is chosen. For that we need to make changes to our whole system of research and innovation.
Marianna Mazzucato, Professor of Economics at UCL and head of their Institute of Innovation for Public Purpose, points out that major advances in technology are rarely made by the private sector. For example all the technology that was used by Bill Gates and Steve Jobs to build the PC and iPhone was developed using government money in the US DARPA programme in the 1960s. In other words the government declared their research objectives, invited interesting projects to be put forward from the widest range of bodies, selected the most promising and funded them. In this way technologies make a leap forward in new and surprising ways. There is then a vital role for companies in developing new products based on those technologies, and they should be encouraged to do so and reap the rewards for so doing. However the government should also earn a return on the earlier investments they have made and currently this is not happening.
This is the exact opposite of the story that we are often told: that governments can’t innovate, that governments make bad investments in new technologies (Concorde is usually mentioned), and that only businesses can be creative. However the full data simply negates this view. Sadly the financial rewards have largely gone to the companies that exploited rather than developed these new technologies (who have then even avoided their fair share of taxation on their profits) but that could be changed so that the government secures a fair return on its investment.
This government-led ‘moonshot’ approach is totally different from todays pharmaceutical research which is cautious and repetitive, and results only in large companies enhancing already large profits without introducing ground breaking new ways forward. So if we are to see this kind of genuinely innovative endeavour we will need the government to take on a much bigger role. This would be even more effective at, say, a European level but it is something that could start with a UK government.
So, as well as a change in the way our NHS is run, a government truly concerned about the health of its citizens would want to tackle this aspect of innovation.
An exciting choice – and the likely reality
The choice
So I suggest we have a choice between a regulated well designed market and an information fuelled centrally directed system but that either of these would benefit from and work well with the kind of ‘moonshot’ approach advocated by Marianna Mazzucato. For such a radical change cross party support would be needed, and maintained through successive parliaments. Thus political parties devising policies will need to think about what package of these will most likely secure cross party support.
My own feeling is that it may be more possible to secure that cross party support for a combination of ‘market and moonshot’, unless it proved possible to convey a vivid enough picture of the way the information driven centrally run system would work. And indeed all three of these systems would need persuasive, eloquent, principled advocates.
Is this likely?
Of course there is only a minuscule chance of this happening. We are much more likely to go on tinkering with the NHS systems in ways that are not understood by the public, and which fail to deliver the care needed.
And that is why it is so important that we all take an active, informed and intelligent interest in what is happening and do not subscribe to sound bites like ‘creeping privatisation’ without fully exploring them and the wider picture.
So do please take a wide and active and informed interest in the NHS – for the benefit of all of us. That will mean listening to a much wider range of voices than healthcare professionals themselves. It means taking an interest in how organisations work, how professionals need both freedom and boundaries, how to approach ‘messes’, and being able to look clearly at the benefits and disbenefits of different kinds of system.
One way of describing this could be a creeping expertise in how a health system ticks – now that would be worthwhile!
![FullSizeRender[3]](http://www.reallylearning.com/wp-content/uploads/2017/08/FullSizeRender3.jpg)

![photo[2]](http://www.reallylearning.com/wp-content/uploads/2015/03/photo2-1024x576.png)